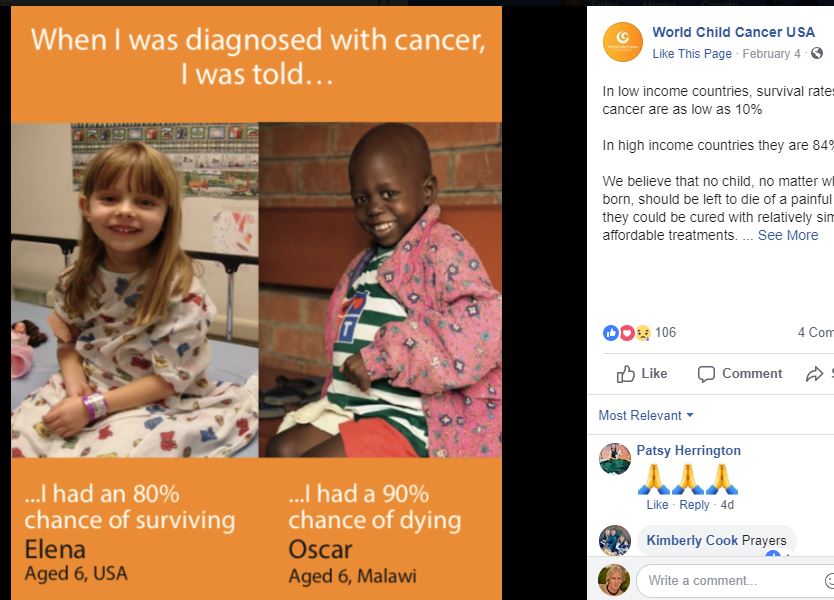
There is a crisis going on; 9/10 kids born in East Africa, diagnosed with cancers, are dying*. Yet that number is 1/10 in the USA. Why? (*Texas Children’s Global Hope program).
Fast facts –
# 18.6% of the world’s pediatric cancers are in sub-Saharan Africa. (More than Europe & North America combined).
# Non-Hodgkin lymphoma & Acute lymphoblastic leukemia are the most common cases of pediatric oncology cases.
# 54% of Kenyan kids abandon their treatment due mainly to finances & travel difficulties.
# W.H.O’s goal, “By 2030, achieve at least a 60% survival rate for childhood cancer globally, and reduce suffering for all.”
So what is Shoe4Africa going to do to play its part? Build sub-Saharan Africa’s 1st Children’s Cancer Hospital.
Background: Meg O’Brien, MD, a member of the American Cancer Society Global Cancer Treatment team, reflects on the stark contrast in cancer treatment between America and Africa. “Since the 1960s, we’ve transformed cancer from a terrifying, virtually incurable disease into something that can be fought and often won. However, this triumph hasn’t extended to Africa,” she laments, highlighting the lack of attention given to cancer care on the continent.
Upon the opening of our primary public children’s hospital in 2015, children were no longer subjected to the chaos of overcrowded adult hospitals, scrambling for bed space. We provided care to children from all walks of life, treating a myriad of diseases. The corridors buzzed with activity, echoing with diverse languages. Yet we never projected how popular the hospital would become and the numbers we would treat.
Despite being nestled in the heart of the Rift Valley, we even extended our care to children from not only all over Kenya, but neighboring countries such as Tanzania, Uganda, Southern Sudan, Rwanda, and even one from Burundi! However, we were aware that our mission was far from complete.
In 2018, a new chapter begins with the story unfolding at the Shoe4Africa Hospital.
Led by Beryl, the goalkeeper wearing green below, our Shoe4Africa team comprises mostly of cancer patients 90%, with only two exceptions. The team were there as we launched a project to install an astro-turf pitch for 5-a-side soccer just outside the hospital building for their use. The joy of taking these patients out to exercise is palpable. Their faces light up with excitement, a testament to the positive impact of physical activity on their well-being. The day was December 31st, 2018.

Team Shoe4Africa. We love you Beryl.

Dr. Kibosia, a highly esteemed figure in Kenya’s medical community, and former CEO of MTRH, once stated, “9 out of 10 children diagnosed with cancer in East Africa do not survive.” In stark contrast, the survival rate in America stands at 1 out of 10. Within our hospital, we witness the grim reality firsthand; our oncology ward typically accommodates 30-40 patients. However, administering chemotherapy in a public children’s hospital poses a significant risk due to the proliferation of diseases. Chemo compromises a child’s immune system, leaving them vulnerable to infections.
Now, Toby, our CEO, is standing looking at his cancer team about to play soccer. He’s thinking of the odds that these little kids face after being born in Kenya.
Recognizing this urgent need, we embarked on a mission to build a dedicated Kids Cancer Hospital, equipped with total isolation facilities to protect these vulnerable patients. Despite receiving encouragement from three esteemed cancer specialists, I hesitated to take action. Surprisingly, no other organization stepped up to address this critical gap in healthcare infrastructure. A search across Sub-Saharan Africa yielded no results – not a single dedicated kids cancer hospital or isolation center.
The solution was clear but daunting: we had to build the Kids Cancer Hospital ourselves. We couldn’t afford to subject children to the risks of infection in conventional hospital settings or send them home where infections were inevitable. Inspired by the proactive approach adopted in the United States, which had significantly improved survival rates, we knew we had to act.
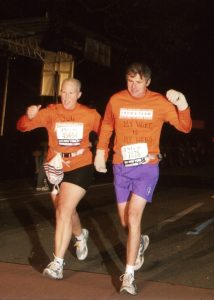
Then, a turning point arrived with the arrival of Doug, who sought to honor his late wife, Juli Anne, a resilient cancer warrior. Juli Anne’s unwavering spirit and her love for Africa motivated Doug to make a substantial donation to kickstart the project. Thus, the hospital found its name – a tribute to Juli Anne’s enduring legacy and her commitment to fighting cancer against all odds.
Juli Anne’s indomitable spirit, as exemplified by her participation in the 2006 New York City Marathon amidst her cancer treatment, continues to inspire us. Her favorite quote, “Never, never, never give up,” embodies the resilience and determination that will drive positive change for children battling cancer in sub-Saharan Africa.
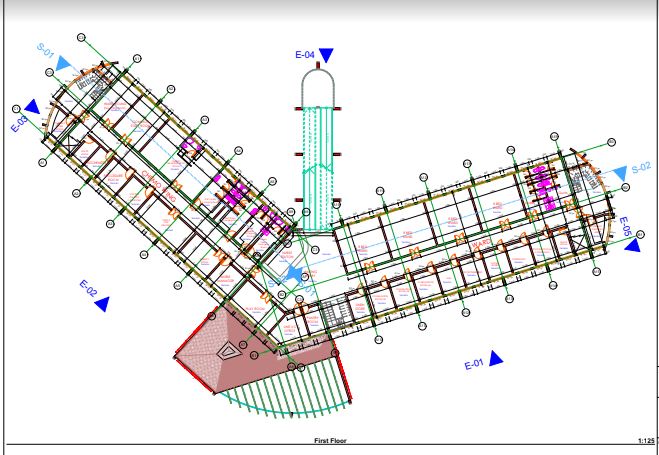
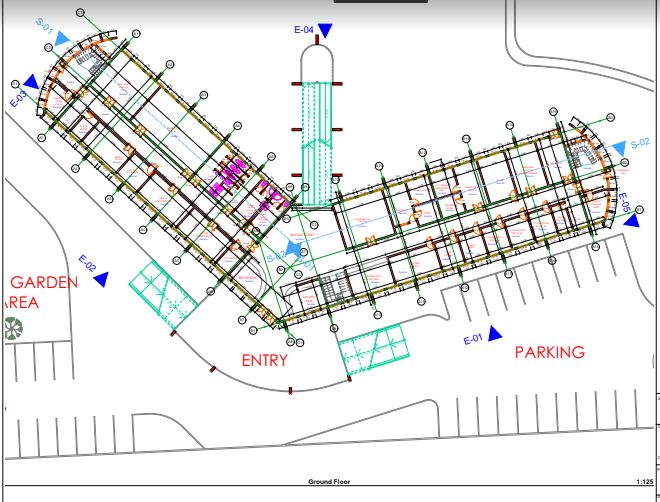
Work in Progress, below
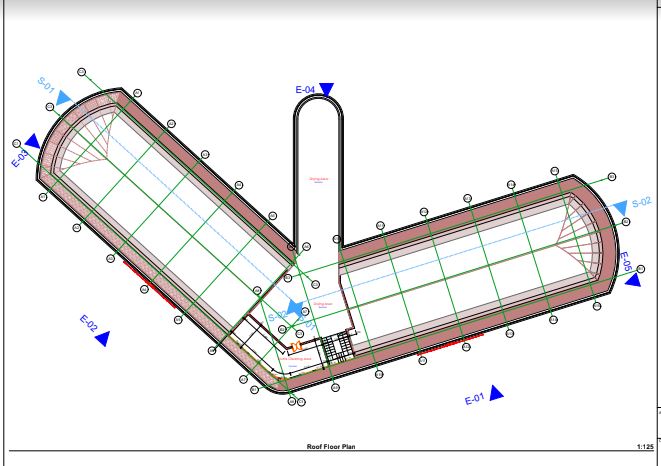
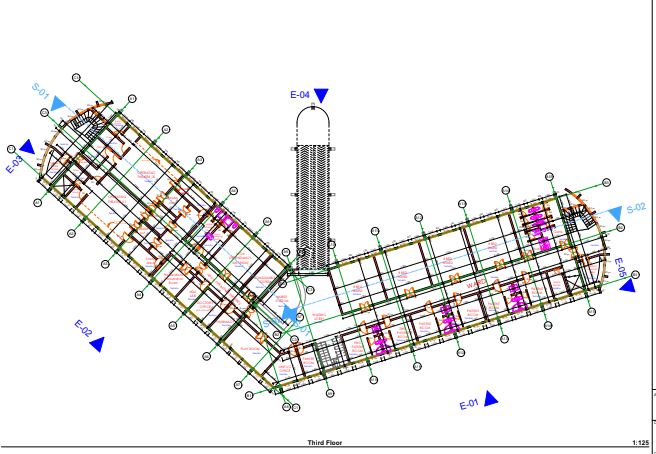
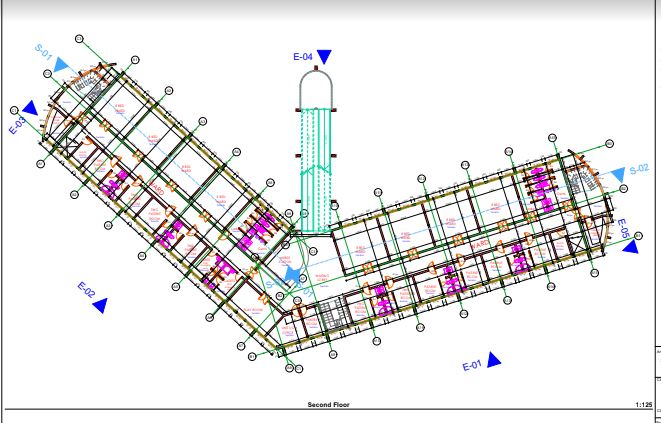
The children’s cancer hospital is designed to accommodate a total of 152 beds, distributed across various wards and rooms to ensure comprehensive care for our young patients.
Here is an overview of the facilities planned for the hospital:
General wards, two-bed, and single-bedded rooms.
Outpatient treatment areas and waiting rooms. Quiet room and teacher’s lecture hall. Doctors lounge and overnight doctors’ room. Resource room equipped with computers. Examination rooms and offices. Main reception and lobby area. Palliative care offices and chemotherapy infusion rooms. Child life therapy and playroom. Research office and units for solid tumors, benign hematology, and malignant hematology. Nursing stations on each floor and Dr’s ward discussion rooms. Common playroom. Pharmacy, medicine mixing area, infusion space, records office, and admission office on the ground floor. Exclusive admission for children under 18 years, with a majority falling between 0-10 years. Radiotherapy administered at Chandaria, while chemotherapy treatment will be provided on-site. Meeting room with a capacity for 100 people, located on the same floor as the lecture room. Ground outpatient area and accommodation for male and female intern doctors overnight. No ICU facilities (to utilize adjacent S4A ICU). Changing rooms for nurses on each floor, with an ideal provision for an exclusive theater if budget permits. Mothers allowed to stay, with provisions for a couch by bedsides but future plan to build a women’s hostel next door.
Our aim is the delivery of state-of-the-art care, training of local healthcare providers, conducting public health campaigns, and establishing a center of excellence for pediatric cancer. And our goals include improving early diagnosis, reducing treatment abandonment, improving the pediatric cancer registry, and offering overall quality services in pediatric oncology.
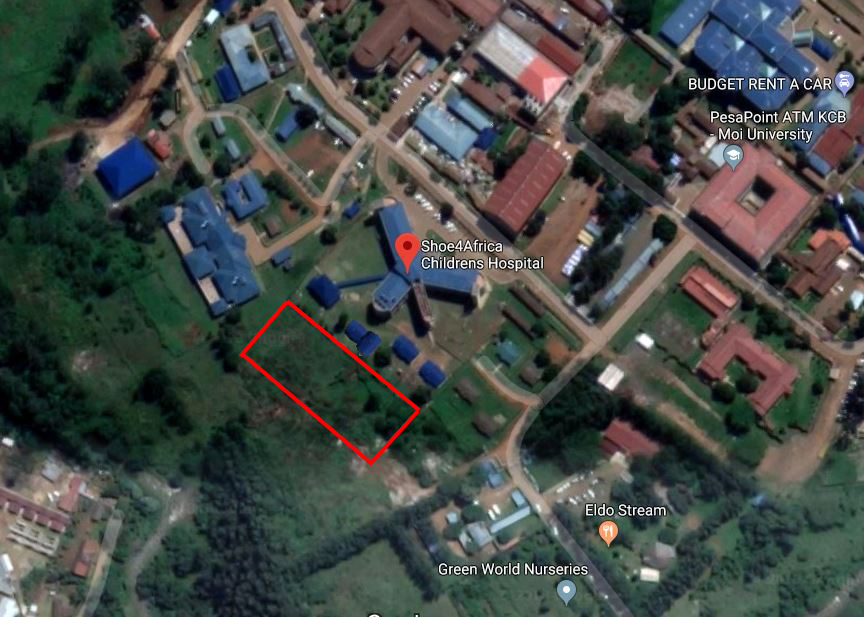
In Kenya there are three Pediatric oncologists who are mainly based in Nairobi. However right now plans are being made to start training Pediatric oncology in Eldoret beginning September 2019 which is about to get approved by Moi University Medical School (2nd largest University in Kenya). The MU Medical school campus is 300-meters from our Hospital (see Map above).
Prof. Gertjan Kaspers, MD PhD Head, Dept of Pediatric Oncology & Hematology, VU Amsterdam, Netherlands. Director of the Academy of the new Dutch Princess Máxima Center for Pediatric Oncology,
“Childhood cancer is the leading cause of death by disease among children in high-income countries. The same will become a reality in other countries such as Kenya, with the improved care of other diseases. However, cancer can potentially be cured in the far majority of affected children. A public childhood cancer center is crucial to care for these patients and to achieve higher cure-rates. I therefore strongly support the activities of Shoe4Africa to help realising such a public center, which would be the first in its kind in Africa”.
Dr. Terry Vik MD Professor, Pediatric Hematology-Oncology, Riley Hospital For Children At Indiana University Health.
“As our resources and capabilities improve, we should see up to 500 patients per year based on the population we serve if this hospital is built. The average length of stay of a newly diagnosed patient is 6-8 weeks, from the time they get admitted to hospital, diagnosed with their cancer, and receive their first course of chemotherapy. The new hospital will be totally isolation disease orientated. Currently, for the four most common cancers seen, lymphoma, acute lymphoblastic leukemia, Wilms tumor, and retinoblastoma, we save about 25% of those children. With better supportive care and new hospital space to reduce infections and abandonment of treatment, we could save over 50% of children. Our goal, once radiotherapy is in place in Eldoret and we implement these improvements, as many as 70% of children should be able to be saved with the therapies we can deliver. If we have a 100 bed hospital and can save up to 350 children per year as a realistic goal. Currently we save about 25-30 children per year in our 24 bed temporary space.”
Dr Festus Njuguna, Childhood cancer specialist at the Shoe4Africa Hospital. “There are 200,000 new cases of childhood cancer annually and 80% of these occur in Lower/middle income countries (LMIC). The LMIC’s account for a staggering 85% of all cancer deaths. The Cancers with poor outcomes usually require isolation treatment, which today is not possible given the current facilities (in Kenya). The new Public children’s cancer hospital is urgently needed.
DR Robert Einterz, is the director of the AMPATH Consortium and director of the Indiana University Center for Global Health. “A pediatric cancer hospital is a critical missing piece in East Africa.”
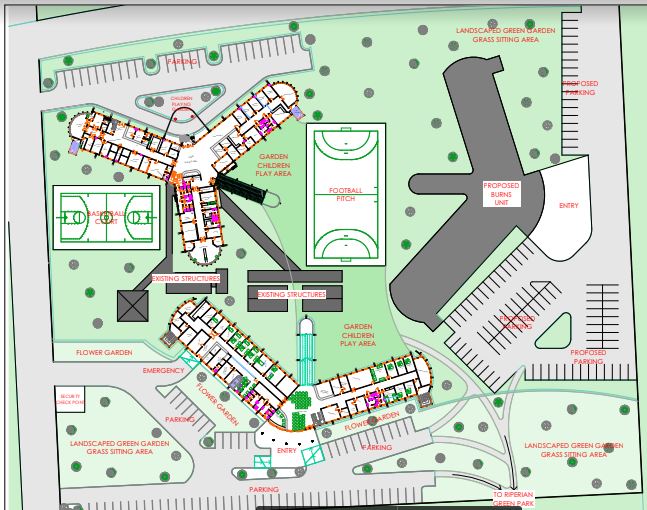
The Campus Map
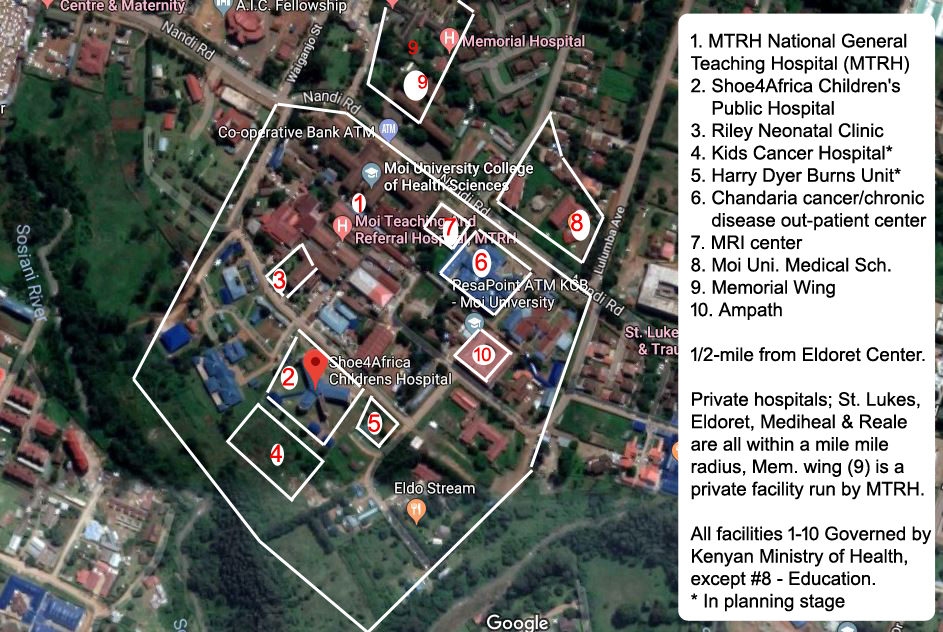
Eldoret, in Kenya, the fastest growing city, with an International airport, on the trunk road between Uganda and Nairobi, our site is situated right in the heart of the city center. Surrounded by a huge public health center, next to one of only two national referral general hospitals in Kenya, next to a Medical school, the location could not be better.

FAQ
When will you start construction? Construction began Jan 2024
Is this Shoe4Africa’s biggest project? No, in 2008 we ‘discovered’ there was not a single public children’s hospital in East & Central Africa. In fact in 2005 Nelson Mandela had pledged that his legacy should be for his foundation to have a children’s hospital down in South Africa, as for the entire region of Sub Saharan Africa (pop. over 1-billion) there was just one; the Red Cross in South Africa. (157 in the USA)
In 2015 we opened the Shoe4Africa Public Children’s Hospital that is today treating 400 patients per day! The Mandela foundation opened in 2017, down in Johannesburg, South Africa. Success! In Dec 2022, we celebrated treating our 1,000,000th patient.
In a sentence… why this project? Because 9/10 kids diagnosed with cancer are dying in East Africa. An isolation specialized kids cancer hospital will be the best solution to immediately start changing this.
How much will this project cost? We are working in two phases; construction is the first phase. For the equipping we already have plans in action, but as this will be in 2022 when the hospital opens we will announce these plans later. But roughly between two point five and three million USD. A similar amount for the equipping.
Where is the expertise coming from? The Kenyan Government will be providing Doctors, and Moi University Medical School (who have a campus 300-meters away from our site!) are planning to start new classes focusing specifically on Pediatric Cancers. We already have interested parties from across the world to partner with us bringing International expertise and have entertained international Doctors at our Children’s Hospital.
Why build so close to the other hospital? Cost saving; building close will mean many duplication’s will not have to be made. There were a number of reasons why we initially picked the site we did for the Children’s Hospital in 2008, and it proved to be the right choice.
Our foundation remains, we believe, is one of America’s most efficient. For 19-years the foundation was run without single salary. We built the kids hospital and 4 schools this way! It is widely understood that 50% of the funds raised for Africa in America are spent in America. If a charity has salaries to pay, and office space in America, it is easy to understand why. Guidestar.org – check out the charities.
Types of common childhood cancers
- Leukemia
- Brain and spinal cord tumors
- Neuroblastoma
- Wilms tumor
- Lymphoma (including both Hodgkin and non-Hodgkin)
- Rhabdomyosarcoma
- Retinoblastoma
- Bone cancer (including osteosarcoma and Ewing sarcoma)
-
Cancer Staging
Staging is the classification of the extent of the disease of cancer. There are several types of staging methods. We will mainly rely on the below numerical system that will often be used to classify the extent of disease.
Stage 0 Cancer in situ (limited to surface cells) Stage I Cancer limited to the tissue of origin, evidence of tumor growth Stage II Limited local spread of cancerous cells Stage III Extensive local and regional spread Stage IV Distant metastases
Site of Cancer Origin
This classification describes the type of tissue in which the cancer cells begin to develop. Here are some common examples of site of origin classification:
- Adenocarcinoma: originates in glandular tissue
- Blastoma: originates in embryonic tissue of organs
- Carcinoma: originates in epithelial tissue (i.e., tissue that lines organs and tubes)
- Leukemia: originates in tissues that form blood cells
- Lymphoma: originates in lymphatic tissue
- Myeloma: originates in bone marrow
- Sarcoma: originates in connective or supportive tissue (e.g., bone, cartilage, muscle)
- Mixed Types: These have two or more components of the cancer.
-
Cancer Diagnosis
A biopsy (removal of tissue for microscopic evaluation) is preferred to establish, or rule out, a diagnosis of cancer.
Usually, a biopsy, along with with advanced imaging technologies, can confirm and locate the presence of cancer in its primary site and secondary sites if metastasized. A cancer’s primary site may determine how the tumor will progress; spread, or metastasize; and may also determine related symptoms that are most likely to occur. A secondary site refers to the body part where metastasized cancer cells develop to form secondary tumors.
The pathologist mainly gives a pathological grade to a tumor according to how malignant the tissue looks under the microscope that will finally confirm the presence of cancer. Cancers are additional classified according to stage.
Here is a posting that we saw on Internet that pretty much shows the need:
Any questions? Please email
More reading on pediatric cancer in Sub Saharan Africa
Global Hope link
Cancer in Children WHO link
Childhood Cancer WHO link
Aslan Project (Ethiopia) link
Site plans and architect sketches